Using mathematical modelling to better understand the role of inflammation in tumour growth

Farjana Aktar
Inflammation can be a healthy process. After an infection or injury, the inflammatory response helps to fight off infection or repair damaged tissue. But when inflammation is long-term (chronic) rather than short-term (acute), it may damage healthy tissues. This is why chronic inflammation is linked to conditions such as heart disease and cancer.
In the case of cancer, inflammation is now known to play a significant role in tumour growth and progression. The power inflammation has in promoting cancer is evident by the fact that anti-inflammatory drugs can lower cancer risk and reduce mortality rates for certain types of cancer, including colon and lung.
It is difficult to adequately quantify systemic inflammation and the resulting localized effects in cancer. Recent master's alumna Farjana Aktar and supervisor, professor Kathleen Wilkie, both of Ryerson’s Department of Mathematics, investigated this problem by using experimental data to infer the possible contributions of inflammation in a mouse model of cancer, with their results published in Mathematical Medicine and Biology (external link) .
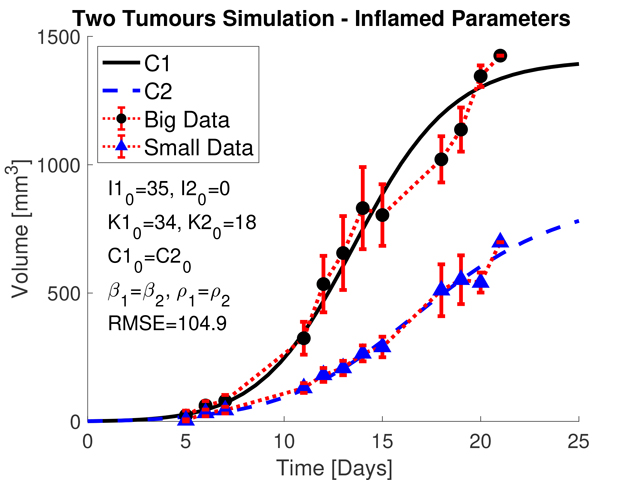
In particular, Aktar’s project focused on explaining an odd experimental observation wherein two simultaneously injected tumours at different sites resulted in many animals with one large and one small tumour. Aktar and Wilkie developed and tested a mathematical model to examine the role inflammation may play in the growth rate separation.
“I explored various scenarios with the mathematical model to determine the most biologically likely set of conditions that could explain the difference in tumour size,” says Aktar. “In the end, I found that the one large tumour/one small tumour phenomenon was likely due to one of the injections being made at a pre-inflamed site due to a pre-existing wound, such as a bruise. The wound caused the levels of inflammatory cells to be higher at that site compared to the other, leading to a larger tumour.”
The team also used their model to explore potential treatment combinations that targeted both the tumour itself (chemotherapy) and the host response (anti-inflammatory and anti-angiogenic treatments that target the immune response and blood vessel growth, respectively). The model predicted that combining all therapies gave the best tumour suppression, highlighting the potential benefit of treating host responses such as inflammation and blood vessel formation in addition to standard anti-tumour therapies.
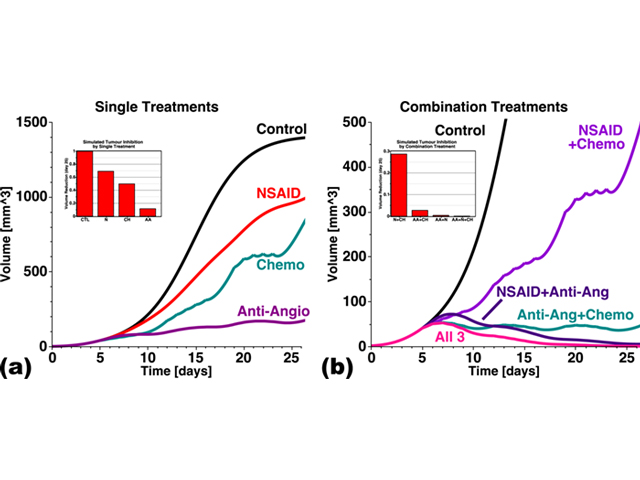
Model predictions of (a) individual treatments (chemo, NSAID and anti-angiogenic therapies) and (b) all possible combinations. Improved tumour control is obtained by targeting both the cancer (chemotherapy) and host (anti-angiogenic and anti-inflammatory). Model simulations of (3.2), (3.4)–(3.6), (3.7)–(3.8) with parameter values listed in Tables 1 and 2
“The paper highlights the importance of inflammation in both the tumour microenvironment and the systemic host environment,” says Wilkie. “The mathematical model is able to link tumours across the body via systemic influences that enable feedback between the tumour sites. This is the first model to directly consider inflammatory effects and anti-inflammatory therapies on tumour growth, and it is carefully parameterized by connecting the model predictions to laboratory experiments at every stage.”
The team’s work suggests that improved tumour control can be obtained by targeting both the cancer and host, through anti-inflammatory treatments, including a reduced metastatic burden after the surgical removal of primary tumours.
The dynamics of the immune response to cancer are nonlinear and often non-intuitive. The mathematical modeling and predictions made in this paper improve our understanding of the influence inflammation has on cancer during both growth and treatment phases.
In her lab, Dr. Wilkie continues to study the interdependent interactions between cancer and the body.
Funding of this research was provided by an NSERC Discovery Grant to Kathleen Wilkie and by the Ryerson Faculty of Science in the form of a graduate student stipend to Farjana Aktar.